One of the concerns that conservatives sometimes bring up is that while it is true that using IVF/ART (in vitro fertilization/assisted reproductive technologies) can have a eugenic effect if they are used with embryo selection, or just plain abortions of fetuses with severe genetic disorders, IVF in general may have a dysgenic effect by helping people have (more) children when nature is indisposed to let them. Consider studies like this one:
- Wang, Y. X., Farland, L. V., Wang, S., Gaskins, A. J., Wang, L., Rich-Edwards, J. W., … & Chavarro, J. E. (2022). Association of infertility with premature mortality among US women: prospective cohort study. The Lancet Regional Health–Americas, 7.
Background Infertility has been associated with common chronic non-communicable diseases. However, the association of infertility with long-term mortality is unclear.
Methods We followed 101,777 women aged 25–42 years at enrollment between 1989 and 2017. Biennial questionnaires updated participants’ infertility status and underlying reasons for infertility throughout their reproductive lifespan. Hazard ratios (HRs) for the associations of infertility with the risk of premature mortality (death before age 70 years) were estimated using Cox proportional hazards models.
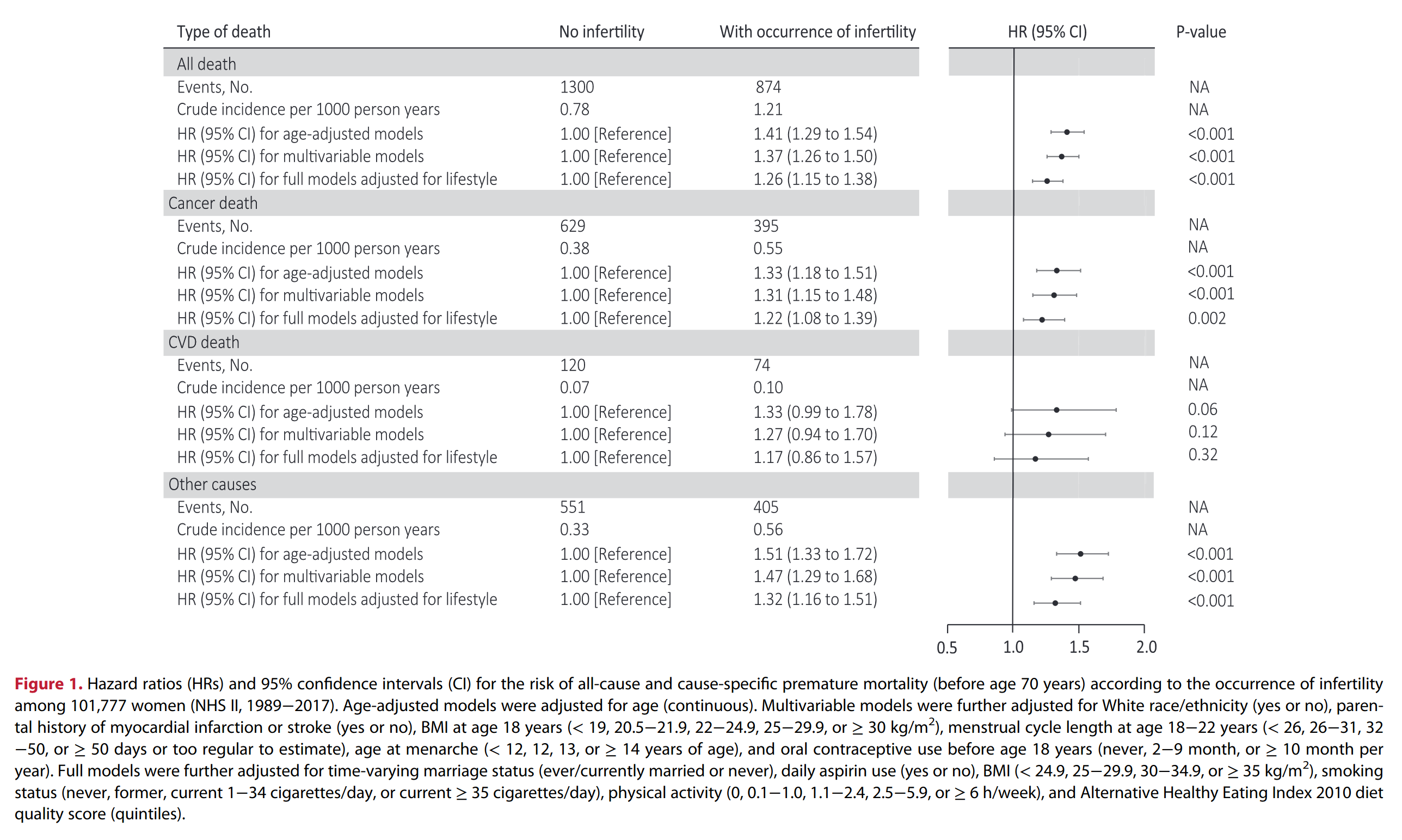
Findings During 28 years of follow-up, 2174 women died before age 70 years. Infertility was associated with an HR of 1.26 (95% confidence interval: 1.15 to 1.38) for premature death. This relation was largely driven by deaths from cancer (HR = 1.22, 1.08 to 1.39) and was stronger among women reporting infertility at a younger age (HR = 1.35, 1.19 to 1.52 for age ≤ 25 years; 1.23, 1.10 to 1.38 for age 26–30 years; and 1.10, 0.91 to 1.32 for age > 30 years, compared to no infertility). The premature mortality risk was also higher for women who didn’t become pregnant after their first report of infertility (HR = 1.39, 1.25 to 1.54) than among women who reported at least one pregnancy after infertility (HR = 1.12, 1.00 to 1.26). When contributing diagnoses of infertility were evaluated, a greater risk of all-cause mortality was associated with infertility due to ovulatory disorders (HR = 1.28, 1.09 to 1.51) and endometriosis (HR = 1.50, 1.22 to 1.83).
- Lindahl-Jacobsen, R., Tavlo Petersson, M., Priskorn, L., Skakkebæk, N. E., Juul, A., Kristensen, D. M., … & Jensen, T. K. (2024). Time to pregnancy and life expectancy: a cohort study of 18 796 pregnant couples. Human Reproduction, 39(3), 595-603.
STUDY DESIGN, SIZE, DURATION A prospective cohort study was carried out on 18 796 pregnant couples, in which the pregnant women attended prophylactic antenatal care between 1973 and 1987 at a primary and tertiary care unit. The couples were followed in Danish mortality registers from their child’s birth date until death or until 2018. The follow-up period was up to 47 years, and there was complete follow-up until death, emigration or end of study.
PARTICIPANTS/MATERIALS, SETTING, METHODS At the first antenatal visit, the pregnant women were asked to report the time to the current pregnancy. Inclusion was restricted to the first pregnancy, and TTP was categorised into <12 months, ≥12 months, not planned, and not available. In sub-analyses, TTP ≥12 was further categorized into 12–35, 36–60, and >60 months. Information for parents was linked to several Danish nationwide health registries. Survival analysis was used to estimate the hazard ratios (HRs) with a 95% CI for survival and adjusted for age at the first attempt to become pregnant, year of birth, socioeconomic status, mother’s smoking during pregnancy, and mother’s BMI.
MAIN RESULTS AND THE ROLE OF CHANCE Mothers and fathers with TTP >60 months survived, respectively, 3.5 (95% CI: 2.6–4.3) and 2.7 (95% CI: 1.8–3.7) years shorter than parents with a TTP <12 months. The mortality was higher for fathers (HR: 1.21, 95% CI: 1.09–1.34) and mothers (HR: 1.29, 95% CI: 1.12–1.49) with TTP ≥12 months compared to parents with TTP <12 months. The risk of all-cause mortality during the study period increased in a dose–response manner with the highest adjusted HR of 1.98 (95% CI: 1.62–2.41) for fathers and 2.03 (95% CI: 1.56–2.63) for mothers with TTP >60 months. Prolonged TTP was associated with several different causes of death in both fathers and mothers, indicating that the underlying causes of the relation between fecundity and survival may be multi-factorial.
Admittedly, it is a somewhat strange measure. If you ask couples who just had a child how long they had been trying for (having sex without protection for the purpose of procreation), they can give you some answer in months or cycles, say 3 months (3rd attempt, since ovulation is the only time pregnancy can occur) or 12 months. If you then check up on the same people much later, you will find that some of them have died. So, in some sense, we have an expectation that general poor health will impact both: making it harder to conceive, and making you die earlier. The studies above tried to quantify this relationship, and indeed, they found that there’s some association. Worse fecundity (ability to get pregnant) relates to higher mortality. This was true for both the fathers and the mothers. This could be interpreted as bad overall health, say, obesity or alcoholism, making sperm quality lower, and various other impediments to achieving pregnancy. But it’s not just that simple, as both studies controlled for a host of other variables, including BMI, and they still find that trying for longer relates to higher mortality.
The presence of the relationship despite numerous controls suggests a more intrinsic relationship, a genetic relationship, since bad health is heritable and so is fecundity (and the resulting fertility). In this way, then, nature is ‘trying’ to improve the genetic quality of the population by the means of making it difficult for unhealthy people to have children. In a natural environment without artificial reproductive technologies, then, there will be some slight eugenic effect of this. Theoretically, then, the increase in the prevalence of ARTs will diminish this natural eugenic effect, by making it more likely that subnormal health couples will have children. From our immediate moral perspective, this is good. Technology is helping couples struggling with a medical issue and to have a family. This is not much different from other medicine, which also saves the lives of some people with poor genetics and allows them to reproduce.
There is one other way that IVF makes dysgenics worse. When natural fertilization occurs, the sperm must first swim through a kind of hostile uterine environment before they make it to the holy grail, the egg. This theoretically imposes some selection on the sperm, making it more likely that the sperm that wins is a quite fit sperm, genetically speaking. In IVF, often a method called ICSI is used, which is when the sperm are too low quality (e.g. can’t swim properly) or too few in number, and so the sperm is placed directly into the egg using a small needle. This is the main treatment for male-related infertility, but again comes at the price of removing a slight eugenic filter effect that exists in nature. In recent years, IVF clinics have been trying out various artificial sperm selection methods to reinstate this eugenic feature. I have a whole blogpost on these methods.
I’ve seen people propose to ban ART/IVF over these slight dysgenic effects, but that is premature. There are other factors to consider. First, ART enables couples to have children later. Since in developed countries, higher human capital couples have children later, mainly due to conflict with education and career demands, ART increases the fertility of such high human capital people, thus having a eugenic effect. We can look up some study to confirm this impression:
Net of education, age, period, and marital status, the incidence rates of ART births are lower for black women (0.57 times; 95% CI, 0.52–0.62) and Hispanic women (0.67 times; 95% CI, 0.57–0.62) relative to white women’s rates; for Asian women, the incidence rates are 1.21 times that of white women’s rates. Further, the incidence rates of ART births are higher for women with more than a 4-year degree (2.08 times; 95% CI, 1.90–2.27) relative to women with a 4-year degree, and are lower for women with less education. Women who are married have an incidence rate of ART that is 5.72 times (95% CI, 5.37–6.09) that of unmarried women. The incidence rates for 2013–2016 are statistically significantly higher than for 2010 by a factor of 1.16 (95% CI, 1.02–1.31), 1.16 (95% CI, 1.03–1.31), 1.27 (95% CI, 1.12–1.43), and 1.51 (95% CI, 1.43–1.82), respectively. The educational differences in ART exist across all age groups from 20 to 49, but are the largest among the 35–39 and 40–44 age groups.
We mainly see what we expect, namely that the higher human capital races use it more (Rushton order: Asian>White>Hispanic>Black), and educated women use it more, but especially so in the later age groups. Thus, we can infer that ART is having a eugenic effect enabling higher fertility among the higher human couples.
Furthermore, banning ART/IVF is very short sighted. The big eugenic gains from ART are yet to come. Polygenic embryo selection (‘PGT-P’) is currently a bleeding edge technology used by the very few people, but it will be mainstream in 10 years or so. This technology allows one to greatly improve human genetic health by avoiding potential children with high genetic risk for many diseases. Since every disease has some heritability, there’s no real limit on how much this can be used. The main problem is that due to the long human generational times, this technology is very slow, even if it was based on perfectly accurate genetic predictions. Of course, the current genetic predictions are not perfect, but they are somewhat better than chance, sometimes a lot better, and that’s a good start.
We don’t really have a choice. Because of genetic mutations that accumulate over time (“mutational load”), and the lack of most of the natural selection from high mortality that we used to have, our collective human gene pool will necessarily deteriorate over time. There are only 2 possible ways to deal with this: 1) go back to high mortality, or 2) some kind of biotechnology. This can be either embryo selection or direct editing (CRISPR-like methods). I think we should stay the course and do as humans have always done, namely to fix problems with technology. We are making rapid progress in both of these directions of biotechnology, and I have no doubt we will make a lot more progress in the future as well.

